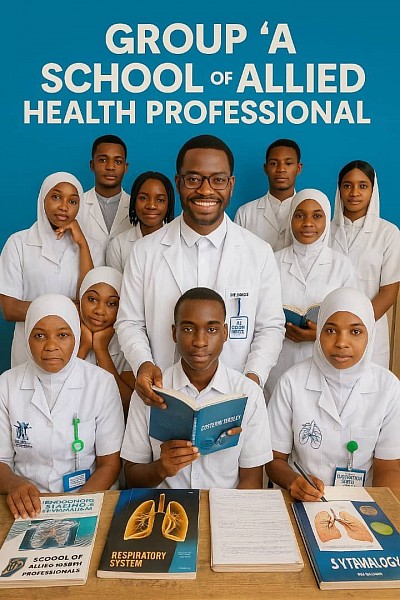
GROUP ''A'' SCHOOL OF ALLIED HEALTH PROFESSIONAL Is a Trademark Of OSB MEDICAL SERVICES AND TRAINING LTD Reg. No:RC2012653.GROUP ''A'' AREA,AWALA ROAD, ISOKAN LOCAL GOVERNMENT APOMU OSUN STATE.
STUDENTS ADMISSION INFORMATION
ADMISSION INFORMATION
Students are admitted twice a year;
(1) January/February Cohort.
(2) June/July Cohort.
SCHOOL ACCOUNT NUMBERS
(1) OPAY: 9035157889 - OSB MEDICAL SERVICES AND TRAINING LTD
(2) MONIE POINT: 9035157889 - OSB MEDICAL SERVICES AND TRAINING LTD.
Elevate Your Career with Allied Health Education
''EVERYTHING YOU WANT IS ON THE OTHER SIDE OF WHAT YOU ARE AFRAID OF,TAKE A BOLD STEP UNDER MORALITY,YOU WILL SURELY GET TO YOUR DESIRED POINTS''
GROUP ''A'' SCHOOL OF ALLIED HEALTH PROFESSIONAL is a clinical skills acquisition institute designed for healthcare workers and those interested in a entry level healthcare profession.We provide a medical education background by skills.Our skills acquisition training training starting from the basic to the most profound.
OUR PROGRAMS
Our program currently is MEDICAL ASSISTANT (Advanced) and carries a professional title of ''MEDIC''
A medic is a person who is trained to provide medical care, especially in emergency situations. Medics can be doctors, nurses, paramedics, or other healthcare professionals. They may work in hospitals, clinics, ambulances, or other settings.
The term "medic" is often used in the military to refer to a soldier who is trained to provide first aid and other medical care to wounded soldiers. Medics may also be deployed to disaster areas to provide emergency medical care to people who have been injured or displaced.
Medics play a vital role in providing healthcare to people around the world. They are often the first people to arrive at the scene of an accident or other medical emergency. Medics are trained to assess the situation and provide immediate care to the injured. They may also transport patients to hospitals or other medical facilities.
Medics are highly trained professionals who are dedicated to providing the best possible care to their patients. They are an essential part of the healthcare system.
The program is programmed to be two years.Students are admitted into CLASS ONE(Basics Medical Study Class),and Students are expected to pass six(6) courses(GASTROENTEROLOGY,UROLOGY, GYNECOLOGY,PULMONOLOGY,BASICS OF EMBRYOLOGY,ANDROLOGY) before catalpult into CLASS TWO(Clinical Study/Practical Class), where student will learn and practice DIAGNOSTIC AND TREATMENT ALGORITHM,and some basics in pharmacology.After a year or more of CLINICAL OBSERVERSHIP and INTERNSHIP, student will sit for the final examination called (CONFIDENCE SCORE EXAM),before receiving his/her Certificate.
GROUP ''A'' SCHOOL OF ALLIED HEALTH PROFESSIONAL CURRICULUM:
*GASTROENTEROLOGY
*UROLOGY
*ANDROLOGY
*GYNECOLOGY
*PULMONOLOGY
*BASICS OF EMBRYOLOGY
*BASICS PHARMACOLOGY
*OBSTETRICS
*GENERAL KNOWLEDGE IN MEDICINE,HEALTH,AND WELLNESS
*AND OTHER MORE TO BE ADDED IN THE NEAREST FUTURE.
PROSPECTIVE COURSES
*CARDIOLOGY(Basics)
*IMMUNOLOGY(Basics)
*HAEMATOLOGY(Basics)
*OSTEOLOGY(Basics)
*ONCOLOGY(Basics)
*NEUROLOGY(Basics)
*PODIATRY (CHIROPODY)
BASICS OF ALLIED HEALTH (What to know about Allied Health)
Allied health professions (AHPs) are a group of health care professions that provide a range of diagnostic, technical, therapeutic, and support services in connection with health care, and which are distinct from the fields of dentistry, medicine, nursing and pharmacy.
In providing care as an AHP, their work may support non-AHP health care roles in providing care, and their work may provide specialty health care that would not otherwise be available.
Allied health and care professionals should not be confused with alternative medicine professionals as Allied Health Professional must work within an evidence based practice model. Additionally, some AHPs may also perform the role of Mid-level practitioners with additional education, training and/or certification. Mid-level practitioners are usually AHPs, nurses or other non-physicians with an extended scope of practice.
Definitionedit
In 2012, the International Chief Health Professions Officers[who?] defined the allied health professions:
Allied Health Professions are a distinct group of health professionals who apply their expertise to prevent disease transmission, diagnose, treat and rehabilitate people of all ages and all specialties. Together with a range of technical and support staff they may deliver direct patient care, rehabilitation, treatment, diagnostics and health improvement interventions to restore and maintain optimal physical, sensory, psychological, cognitive and social functions.[1]
Professionsedit
Generally, AHPs provide health and care services which are distinct fields of study from non-AHP health care professions. There will generally be a large demand for professionals in their respective fields and these professions will usually require specialised training, higher level education and certification/licensure which will usually prevent it from being an extension of medicine or nursing roles. AHP roles are usually subject to statutory regulation and registration due to their ability to perform some, specific, restricted medical actions.
Depending on the country and local health care system, a limited subset of the following professions (professional areas) may be represented, and may be regulated:
Anesthesia technicianAnesthesiologist assistantArt therapist / art psychotherapistAthletic trainerAudiologistAutotransfusionistCardiovascular technologistClinical neurophysiologyClinical officerCommunicative disorders assistantDental assistantDental hygienistDental therapistDenturist / clinical dental technicianDietitian / nutritionistEnvironmental health officer / public health inspectorExercise physiologistHealthcare technicianLactation consultantMedical assistantMedical interpreterMedical laboratory professionalsMedical radiation scientistMental health counselorMidwifeMusic therapistOccupational therapistOperating department practitionerOrthoptistOrthotist / prosthetistParamedicPedorthistPerfusionistPharmacy technicianPhlebotomistPhysiotherapist / physical therapistPhysician AssistantPhysician AssociatePsychologistRadiographer (or radiology technologist; includes specialist radiographers, e.g. angiographer, mammographer, etc.)Radiotherapist / radiation therapist / medical dosimetristRecreational therapistRehabilitation counselorRenal dialysis technologist[2]Respiratory therapistSonographer (often, but not always, state-registered radiographers)Speech and language pathologistSurgical technologist
The precise titles, roles and requisites of allied health professionals may vary considerably from country to country. A generic definition for the United States is in the Public Health Service Act.[3]
Other healthcare professionsedit
Depending on jurisdiction the professions that are considered AHPs vary.
AHPs are generally considered distinct from other healthcare service providers on the basis of several factors. These factors may include AHPs offering services that support the treatment of service users in ways which support treatments provided by other health care professionals, or by providing services which other health care professionals require and cannot provide themselves. Additionally, areas of allied health care are generally large and specialised areas which are require specific training and/or certification. Moreover, some professions may be arguably be considered AHPs simply on the basis of their smaller size proportional size to other professions such as medicine and nursing. These factors in combination are likely the cause of differences in regulation and inclusion across jurisdictions.
For example, the United States Association of Schools of Allied Health Professionals[4] uses wording from the Public Health Service Act to list those who are and are not allied health professionals in the United States.[3] Those professionals who are excluded are those who possess degrees, or an equivalent degree, in the following:
ChiropracticClinical psychologyCounselingDentistryHealth administrationMedicineNursingOptometryOsteopathic medicinePharmacyPhysician assistantPodiatryPublic healthSocial workVeterinary medicineTraining and educationedit
Some allied health professions are more specialized, and so must adhere to national training and education standards and their professional scope of practice. Often they must prove their skills through degrees, diplomas, certified credentials, and continuing education. Other allied health professions require no special training or credentials and are trained for their work by their employer through on-the-job training (which would then exclude them from consideration as an allied health profession in a country like Australia). Many allied health jobs are considered career ladder jobs because of the opportunities for advancement within specific fields.[5]
Allied health professions can include the use of many skills. Depending on the profession, these may include basic life support; medical terminology, acronyms and spelling; basics of medical law and ethics; understanding of human relations; interpersonal communication skills; counseling skills; computer literacy; ability to document healthcare information; interviewing skills; and proficiency in word processing; database management and electronic dictation.[6]
Historyedit
The explosion of scientific knowledge that followed World War II brought increasingly sophisticated and complex medical diagnostic and treatment procedures. Increasing public demand for medical services combined with higher health care costs provoked a trend toward expansion of service delivery from treating patients in hospitals to widespread provision of care in physician's private and group practices, ambulatory medical and emergency clinics, and mobile clinics and community-based care. In the developing world, international development assistance led to numerous initiatives for strengthening health workforce capacity to deliver essential health care services. What followed has been an increase in the need for skilled health care delivery personnel worldwide.
Changes in the health industry and emphasis on cost-efficient solutions to health care delivery will continue to encourage expansion of the allied health workforce.
NOTING IS IMPOSSIBLE TO ARCHIVE THROUGH STUBBORNNESS UNDER MORALITY.